What Do You Mean BMI and My Weight are Not the Most Important Measures of My Health?

Answer Provided by David C. Voellinger, MD, FACS, FASMBS, DABOM
Spring 2019
“What do you mean, you don’t want me to lose weight?”
This was my patient’s reply when I told her it wasn’t weight- loss that was most important after her bariatric surgery. She looked at me like I had gone crazy. I could see her thinking, “Dr. V, you may need a doctor’s appointment yourself.”
Like most patients, she was fixated by the number on the scale. Sometimes she would weigh herself multiple times each day, even though my team stressed only weighing-in once a week at most. Sadly, we even reinforced her belief. What was the first thing she did every time she came to our office? We weighed her. Not only did we document her weight each visit, but we also always talked about “BMI,” an acronym all our patients know stands for Body Mass Index. BMI is a measure for the severity of her disease, as well as the measure of her risk for obesity-related conditions like high blood pressure, sleep apnea, high cholesterol or heart disease. It was even the measure of her success following her bariatric surgery. Everything we did revolved around the number on the scale and her calculated BMI.
Insight on BMI, Weight-loss and Obesity
The reality is that, as the Centers for Disease Control (CDC) says, “BMI is only a screening tool and not diagnostic of body fat or the health of an individual.” It does allow us to “categorize” weight issues into classes of underweight, healthy weight, overweight, obesity and severe obesity to allow for comparison studies. It can be confusing as we all know people with a normal BMI who are unhealthy. For example, someone with a BMI of 25 can suffer from high blood pressure or high cholesterol due to a genetic predisposition to the disease. We also know people with high BMIs who are healthy, like an NFL linebacker with a BMI of 37 due to their high amount of muscle mass.
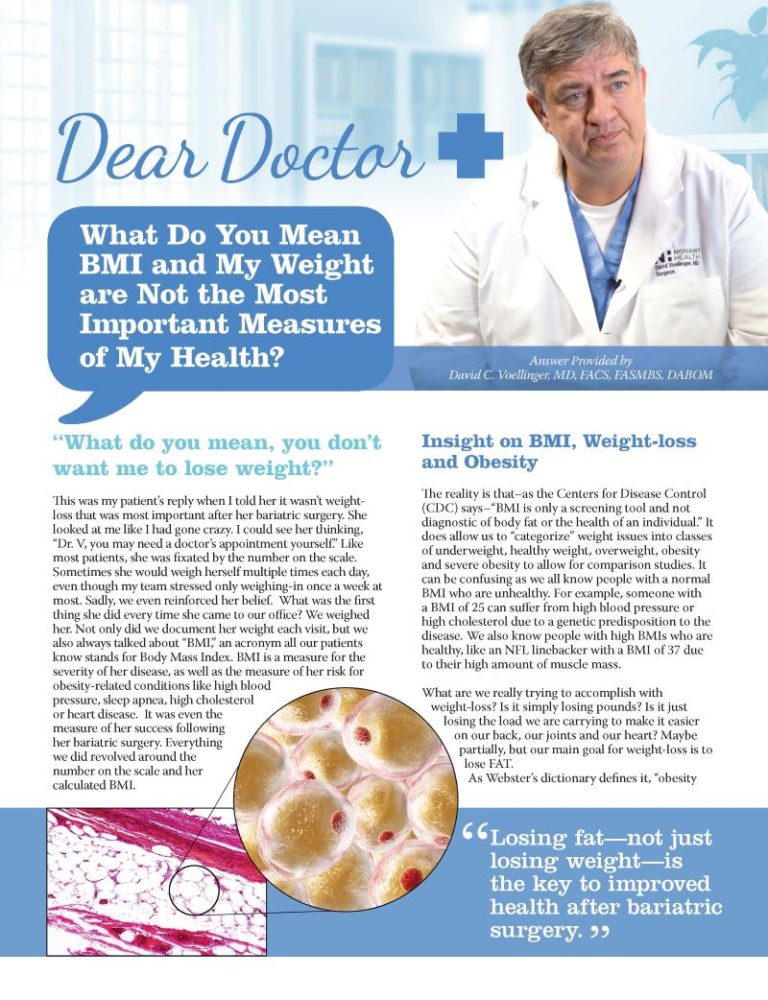
What are we really trying to accomplish with weight-loss? Is it simply losing pounds? Is it just losing the load we are carrying to make it easier on our back, our joints and our heart? Maybe partially, but our main goal for weight-loss is to lose FAT.
As Webster’s dictionary defines it, “obesity is a condition characterized by the excessive accumulation and storage of fat in the body.” Or, even better (and fancier) is the Obesity Medicine Association definition: “obesity is a chronic, relapsing, multifactorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences.” Put simply, all of this means that too much fat in our fat cells creates abnormal, poorly functioning cells that cause inflammation and obesity-related conditions. Losing fat — not just losing weight — is the key to improved health after bariatric surgery.
Beyond Losing Fat: Gaining Muscle
Truthfully, improved health through weight-loss goes beyond that. Not only do we want to lose fat, but we also want to maintain or (ideally) build muscle.
Muscle, also known as lean body mass (total body mass minus fat mass) is essential for support, mobility, strength and endurance. Lean body mass is also important for body metabolism or Basal Metabolic Rate. Having more lean body mass results in a higher metabolism. Unfortunately, when you lose weight after bariatric surgery, an average of 20 percent of your total weight lost is lean body mass — not fat mass. Therefore, it is extremely important to consume enough protein and exercise regularly to maintain or rebuild muscle. You will not only burn more calories, but you will also maintain or even improve your metabolism!
You should know that exercise comes in two forms:
- Cardiorespiratory (cardio): Exercise that raises your heart rate and keeps it up for a prolonged period of time, also known as aerobic exercise.
- Resistance: Exercise that increases muscle strength by making your muscles work against a weight or force.
The American College of Sports Medicine recommends five days of moderate intensity cardio and at least two days of resistance training each week.
Understanding Body Composition
How can you find out your fat mass and muscle mass? In our office, we believe the measurement of your body composition is as important — if not more important — than your weight on a scale. We use a validated four-compartment medical Body Composition Analyzer with an open design, large platform and handrails that make the procedure comfortable and quick — just like stepping on a scale. Every patient receives a baseline body composition analysis followed by a six-month and a 12-month test.
With this information we can determine:
- Is the patient losing an appropriate amount of fat mass?
- Is the patient losing too much lean body mass?
- Are there certain areas of the body that need to be particularly targeted?
We use this information to customize each patient’s eating plan and exercise regimen with the help of our dietitians and athletic trainers. Doing this takes the focus off the scale and places it on the patient’s overall body composition for a more accurate representation of each patient’s progress. It’s also a great motivating tool.
Conclusion
As I ultimately explained to my patient, what is most important is not weight-loss but fat loss and maintaining or increasing lean muscle mass. Body composition is way more important that any number on a scale. Weight will always be important in monitoring trends and as a screening tool. However, to provide the best indicator of your health, let’s step up on our Body Composition Analyzer and see what’s really going on. The light bulb went off and she looked at me like I wasn’t really crazy after all.
About the Author:
David C. Voellinger, MD, FACS, FASMBS, DABOM, is the Lead Physician at Novant Health Bariatric Solutions located in Charlotte, Huntersville, Matthews and Ballantyne. He is also the Medical Director of the Novant Health Bariatric Center.
Post-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View VideoIt can be challenging to find the right help for your child who has obesity. The first…
View VideoConsidering a robotic surgery procedure? In this Health Talk, you’ll hear from bariatric surgeon Walter Medlin, MD,…
View Video