Weight-loss Surgery Abroad: Traveling Toward Disaster?

By Julie M. Hill-Janeway, BBA, MSA, JD, ABD/PhD & Karen Sparks, BBA, MBEd
Summer 2008
Treatment for morbid obesity and related diseases is no longer limited to western nations, and patients seeking bariatric surgical treatment are no longer limited to their own borders. What patients cannot get domestically, they will get internationally.
Patients are flocking to other countries for everything from dental care, to state-of-the-art hip resurfacing. Patients are also flying off to foreign lands seeking weight-loss surgery in increasing numbers – and most of the time all they are buying is a plane ticket and box full of trouble.
Medical Tourism
It’s called medical tourism. Medical tourism, (also called medical travel or health tourism), is a term initially coined by travel agencies and the mass media to describe the rapidly-growing practice of traveling to another country to obtain healthcare.
A growing number of tourists are combining holidays with healthcare, and that is because a growing number of countries are offering expensive and inaccessible or unobtainable medical care at third-world prices.
Some of these individuals either cannot afford the treatment they need at home (for the uninsured), while others are going for procedures not covered by their insurance, such as weight-loss surgery (which includes adjustable gastric band surgery and gastric bypass) and attendant plastic surgery for body-re-contouring.
Medical tourism trends continue to grow every year. Medical tourism is expected to be a global $2 billion dollar market by 2012. The informal channels of communication and scheduling between medical service provider and customer often have no contracts and little information about, or connection with, each other.
This type of loose arrangement means less regulatory or legal oversight to assure quality and competence, and less formal recourse to reimbursement or redress. Not only is there very little in the way of agreements or defined expectations, but the potential for disagreement or disaster can lead to attempted litigation in a foreign jurisdiction.
Why People Go Abroad for Medical Treatment
A large draw for medical travel is convenience and speed. Countries that operate public healthcare systems are often so taxed that it can take considerable time to get non-urgent medical care. The time spent waiting for a weight-loss surgery procedure in Canada can be anywhere from three to eight years, and gastric banding is not covered at all. Patients must pay out-of-pocket for the banding procedure, and for all pre-care and follow-up care as well.
In contrast, in Mexico, Brazil, Germany, Thailand, Cuba, Colombia, the Philippines, or India, a patient could feasibly have an operation the day after arrival, and in many cases for one quarter to one sixth of the price at home. The rate at which you can get it set up and paid for determines how fast you can have your surgery. Supply and demand – capitalism is alive and well outside the United States.
Perceptions of Going Abroad for Treatment
Perceptions of medical tourism are not always positive. In places like the U.S., which has high standards of quality and regulatory agencies and oversight organizations to help insure competence and experience, medical tourism is viewed as risky.
While the tourism component might be a big draw for some Southeast Asia countries that focus on simple procedures, India is positioning itself as the primary medical destination for the most complex medical procedures in the world – including weight-loss surgery. India’s commitment to this is demonstrated with a growing number of hospitals that are attaining the U.S. Joint Commission International (JCI) accreditation to help capture the U.S. medical tourism market.
What Consumers Should Know
But do not think that it is just that easy. This should not be an “if you build it, they will come” scenario. There are other issues to consider and most of them will lead right back to your safety and your well-being pre and post-surgery.
Standards, processes, regulation and oversight are everything when it comes to watch-dogging medical care. The medical tourism consumer has no way to determine whether the facility and provider with whom they are scheduling has any more experience, training or even familiarity with the procedure than they state they have. In most cases there are no public documents that can be checked and no regulatory agencies that can be consulted.
There is not even really any way to check whether they actually know how to do a minimally invasive surgery or whether they have appropriate tools and equipment with which to perform it. You may be expecting six little wounds and wake up with 12-inch long incision. Too late now…
Additionally, there is no way to check if the hospital or surgical facility is in compliance with the standards we would expect from a U.S. surgical facility, or whether the equipment being used dates from any time after WWII.
- Does the facility have appropriate emergency and
back-up measures and systems like an emergency
room or critical care facility? - Are they using black market implants, medications, surgical implements and other materials or equipment?
- Are the medications, supplies and other materials outdates, recalled, expired or stored correctly?
- Is the surgical suite really sterile, or is it just separated from the waiting room by plastic sheeting?
What this All Means
In considering leaving the country for medical treatment, the types of concerns stated above have crossed the minds of many. The answer for these patients has been to stay away from the more “exotic” countries, and seek treatment in Europe which is perceived to have the same, or relatively close standards in treatment and care, as the U.S. or Canada. Although Europe has shown itself to be a world leader in some areas of medicine, it is not necessarily a world leader in all areas of medicine. So, be very careful in generalizing about where you are going in relation to the type of treatment you are seeking.
It is Not Just about the Surgery
For weight-loss surgery patients, there are a number of other concerns and considerations that should be taken into serious account before booking a medical tourism jaunt. First and foremost, weight-loss surgery is NOT just about the surgery. In fact, any experienced and trained bariatric surgeon will tell you that it is really only worth about 10 percent of the success equation. The other 90 percent is found in the pre-care, the education, the skill training, the support portion, the follow-up care, and the behavior and lifestyle changes, among others.
When a patient seeks surgery out of the country, there is usually little to no pre-surgery care, screening, testing/evaluation, education or skill training simply because there is not time in the trip or in the schedule. Appropriate pre-surgical programs can take anywhere from two weeks to six months (excluding patients with particular issues that require treatment longer than six months). Patients are often not even asked, let alone required, to submit medical records for evaluation and consideration. The pre-surgical work-up, evaluation and training are almost universally missing in medical tourism, and patients may never even see a behaviorist, an internist, an exercise physiologist or a dietitian.
And speaking of dietitians… even if a patient does have a nutrition consult, that is all it is – a consult. There is no ongoing nutritional support, evaluation and education. Additionally, not all dietitians in the U.S. are required to be licensed or certified, and virtually anyone can call themselves a nutritionist. In other countries, there is no guarantee that the “dietitian” has any formal training at all, especially as it relates to obesity and bariatric surgery.
The dietitian may also have developed a food protocol based on the local cuisine, customs, lifestyle and food availability and that may not translate at all to the patient’s home environment. The patient could be left with little direction on what to eat, what not to eat, and when and how to eat it.
Finally, the dietitian may not be able to give the patient any useful advice or resources on appropriate bariatric vitamins or supplements that are/may be necessary to achieving healthy nutritional status. The education, evaluation and support will simply be missing, and setting the patient up for post-surgical failure.
So, you see? It’s not an, “if you build it, they will come,” scenario. There is a lot to consider. How about this consideration: some countries, such as India, Malaysia, Costa Rica or Thailand have different infectious diseases than Europe and North America, or different prevalence rates than Western Europe, the U.S. or Canada. Patients who have not had years to build up resistance or tolerance to these diseases are at serious risk for exposure, especially when they are in a weakened state such as with the immune system compromise that often accompanies morbid obesity, or the weakened state that follows surgery.
Of special concern is exposure to gastrointestinal diseases (i.e. Hepatitis A, amoebic dysentery, paratyphoid), mosquito-transmitted diseases, influenza, and tuberculosis (i.e., 75 percent of South Africans have latent tuberculosis). Has that crossed your mind?
Post-care Considerations
Not all the problems stem from lack of appropriate pre-care, though. Other post-care questions and concerns rear their ugly little heads as well.
- Who will do my blood tests?
- Can I find a practice at home that will let me come to their support group?
- Do I understand the importance of a support group?
- Who will do my band fills?
- If I have emotional difficulties, who will see me for these?
- How will I find reliable resources and educational materials?
- What if I have a complication, who will see me?
- What if I develop adhesions or a hernia – will a surgeon take on my case to help me?
- Can I trust that an emergency room in my community will know how to treat me, especially if I arrive unconscious and unable to relay my situation?
- Who will monitor my nutritional status?
- What if I need medications for specific issues related to my obesity or my surgery? Who will I see for that?
- Will I be made aware of what I am supposed to do following surgery, when I am supposed to do it, for how long, why I am supposed to do it, and how it will help me?
- Will there be a language barrier I have to overcome in trying to get information?
- What if I begin to put the weight back on? Who will help me then?
Traveling Back Home Post-Surgery
Finally, consider that patients often travel long distances on planes shortly after surgery. Air travel severely limits a person’s ability to walk around, and the cabin is pressurized, both of which can seriously contribute to the formation of a deep venous thrombosis in the leg, which can quickly become a fatal pulmonary embolism (PE). If this happens mid-flight, no matter how many doctors are on board, they won’t be able to save you.
If you decide to stay in a warm, exotic climate and lay in the sun to heal, well good for you. You may decrease your chances of getting a fatal PE. But remember, scars will be darker and more noticeable if they sunburn while healing. So maybe that is not such a great option either.
Your Options
As you can see, patients have much to consider when choosing their treatment option. One of your best options may be to continue fighting for coverage for your obesity treatment, surgical or not. Keep researching for options within the U.S. Keep attempting to manage your obesity the best you can in the mean time, and do not let your desperation get the better of you and send you from the frying pan into the fire.
Many of us are working tirelessly to bring you coverage and access to appropriate medical care so you do not ever have to think about going out of the country in order to try and save your own life. If after reading all this, you are still considering medical travel, then remember: you get what you pay for. Aren’t you worth the best? We know you are.
About the Authors:
Julie Janeway, BBA, MSA, JD, ABD/PhD, is a gastric bypass patient and co-author of the best-selling book The REAL Skinny on Weight-loss Surgery: An Indispensable Guide to What You Can REALLY Expect! – 2nd edition. Ms. Janeway is a college professor and public health and bariatric educator who teaches patients, medical professionals and others all over the country. Ms. Janeway is a member of the OAC Board of Directors.
Karen Sparks, BBA, MBEd, is a gastric bypass patient and co-author of the best-selling book The REAL Skinny on Weight-loss Surgery: An Indispensable Guide to What You Can REALLY Expect! – 2nd edition. Ms. Sparks is a college professor and public health and bariatric educator who teaches patients, medical professionals and others all over North America. Ms. Sparks is a member of the OAC Advisory Board.
Resources:
www.globalsurgerycenter.com/tour.html
www.cbsnews.com/stories/2007
Medical Tourism Growing Worldwide, by Becca Hutchinson, UDaily, July 25, 2005.
Health Tourism 2.0., World Health Tourism Congress.
Medical Tourism: Need Surgery, Will Travel, CBC News Online, June 18, 2004.
Indian Medical Care Goes Global, Aljazeera.Net, June 18, 2006.
India – The Emerging Global Health Destination, by Suzanne Maguire, Ezine Articles, 2007.
Medical Tourism: Hidden Dimensions, by Rabindra Seth, Express Hospitality, June, 2006.
Vacation, Adventure, and Surgery?, CBS News: 60 Minutes, September 4, 2005.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
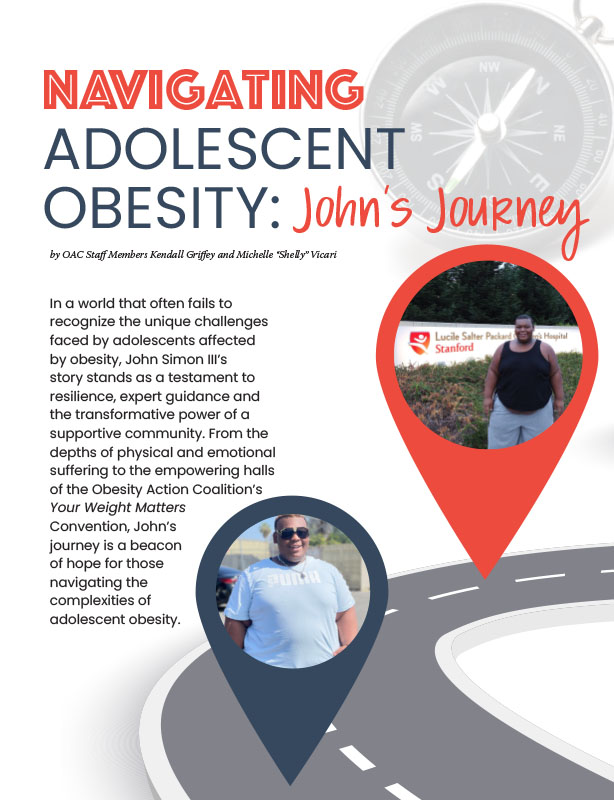
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article