Obesity and Gallstones- How Are They Related?

by Jennifer Franceschelli Hosterman, DO
Spring 2017
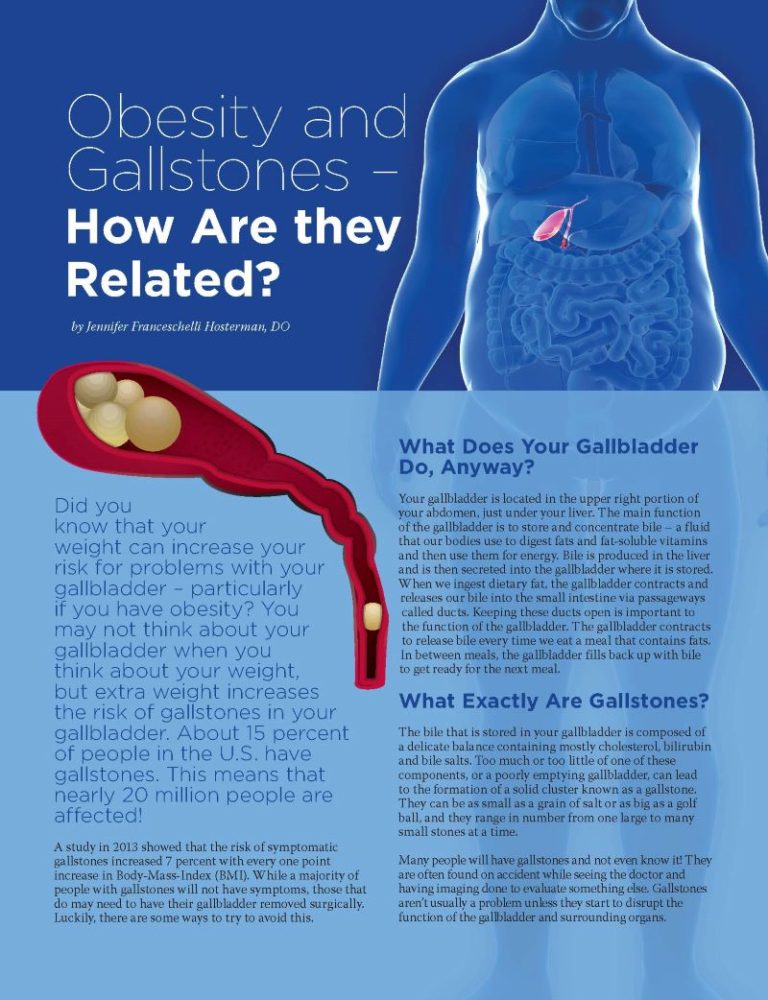
Did you know that your weight can increase your risk for problems with your gallbladder – particularly if you have obesity? You may not think about your gallbladder when you think about your weight, but extra weight increases the risk of gallstones in your gallbladder. About 15 percent of people in the U.S. have gallstones. This means that nearly 20 million people are affected!
A study in 2013 showed that the risk of symptomatic gallstones increased 7 percent with every one point increase in Body-Mass-Index (BMI). While a majority of people with gallstones will not have symptoms, those that do may need to have their gallbladder removed surgically. Luckily, there are some ways to try to avoid this.
What Does Your Gallbladder Do, Anyway?
Your gallbladder is located in the upper right portion of your abdomen, just under your liver. The main function of the gallbladder is to store and concentrate bile – a fluid that our bodies use to digest fats and fat-soluble vitamins and then use them for energy. Bile is produced in the liver and is then secreted into the gallbladder where it is stored. When we ingest dietary fat, the gallbladder contracts and releases our bile into the small intestine via passageways called ducts. Keeping these ducts open is important to the function of the gallbladder. The gallbladder contracts to release bile every time we eat a meal that contains fats. In between meals, the gallbladder fills back up with bile to get ready for the next meal.
What Exactly Are Gallstones?
The bile that is stored in your gallbladder is composed of a delicate balance containing mostly cholesterol, bilirubin and bile salts. Too much or too little of one of these components, or a poorly emptying gallbladder, can lead to the formation of a solid cluster known as a gallstone. They can be as small as a grain of salt or as big as a golf ball, and they range in number from one large to many small stones at a time.
Many people will have gallstones and not even know it! They are often found on accident while seeing the doctor and having imaging done to evaluate something else. Gallstones aren’t usually a problem unless they start to disrupt the function of the gallbladder and surrounding organs.
You might begin to experience symptoms if they get stuck in the ducts and bile cannot get out of the gallbladder. This buildup of pressure in the gallbladder can be uncomfortable and even painful, and it’s often referred to as a gallbladder attack. Attacks are usually triggered by a fatty or heavy meal. Symptoms usually last for the time that the gallstone is blocking the duct, and they go away once the duct is no longer blocked. This can be for several minutes to several hours, but if the gallstone does not dislodge, it can cause serious side effects like infection, inflammation and dehydration.
What Does My Weight Have to Do with Gallstones?
Why does my weight matter?
Obesity – At least least 25 percent of individuals with severe obesity (BMI > 40) have evidence of gallstone disease. Where you carry this extra weight also makes a difference. Scientists believe that your risk is even higher when you carry more of this extra weight around your abdomen than in your hips and thighs. However, adults are not the only ones affected. A study in 2012 noted that children with overweight or obesity were more likely to have gallstones compared to those who were underweight or at average weight. Obesity in the late teenage years seems to carry the highest risk.
One of the many concerns linking obesity and the gallbladder is that obesity can make it harder for the gallbladder to empty. Bile then becomes stagnant and more concentrated, which in turn increases the chances of precipitating a gallstone. Another concern is that obesity is associated with increased cholesterol production in the liver which leads to more cholesterol in the bile. This disrupts the balance of bile composition and therefore increases the risk of gallstone formation.
Rapid Weight-loss/Bariatric Surgery – Rapid weight-loss is defined as losing more than three pounds per week, and it’s also associated with an increased risk of gallstone formation. One explanation for this is the increase in mobilization of cholesterol from fat tissue during the rapid weight-loss phase. This, in turn, leads to more cholesterol in the bile – thus causing the imbalance that can lead to gallstones.
About 30 percent of people within 12-18 months after bariatric surgery will develop new gallstones. People with gallstones related to weight-loss are more likely to have symptoms compared to those without rapid weight-loss.
Low-calorie Diet or Prolonged Fasting – Nearly 10-12 percent of people on a low-calorie diet for 8-16 weeks will develop gallstones. The gallbladder contracts when we ingest fats. If you are on a very low-calorie diet or you’re fasting for a long period of time, then little (if any) fat is ingested. This is because the gallbladder doesn’t have to contract and empty itself regularly, leaving gallstones subject to form.
Weight-cycling – Repeatedly losing and gaining a significant amount of weight can also increase your risk of gallstones, but the reason is unclear. The rise in cholesterol associated with rapid weight-loss may be the culprit. Additionally, some yo-yo dieting requires prolonged fasting which is also a likely contributor.
Physical Activity – Having a more sedentary lifestyle can be associated with a higher risk of gallstones. The reason for this may have to do with the increase in weight that often occurs if we are less active.
Non-weight-related Risks for Gallstones – Being over 40 or being a female can increase your risk for developing gallstones substantially. Pregnancy, family history of gallstone disease and even some medications are other factors known to increase the incidence of gallstones.
What Are the Treatment Options?
Observation – Having gallstones does not mean that you need your gallbladder removed right away. A majority of people with gallstones will never have any symptoms. In this case, people are monitored and they should be aware of potential symptoms so that they can notify their doctor if any develop.
Medical Treatment – There are medications that can help to dissolve the gallstones. These work on smaller gallstones and may take months or sometimes years to work. However, there is a chance that the stones will reoccur once the medication is stopped.
Surgical Treatment – If you are experiencing serious/chronic symptoms such as fever, vomiting, jaundice (yellowing of the eyes/skin) or low blood pressure, then your doctor may recommend that you have your gallbladder removed. This is called a cholecystectomy, and it’s often done laparoscopically (several small incisions in the abdomen instead of one larger incision). After this procedure, most people can go home that very day. If symptoms
are more severe or the surgeon has to do an “open” cholecystectomy (a much larger incision instead of several smaller incisions), then you may stay overnight in the hospital for a few days to ensure a healthy recovery.
What Can You Do to Reduce Your Risk?
Maintain or Strive Toward a Healthy Weight – If you are losing weight rapidly (> 3 pounds per week) or have had weight-loss surgery, then you should talk with your doctor about your own individualized risk reduction plan. If possible, aim to make more gradual changes with a weight-loss goal of about ½ -2 pounds per week.
Avoid “Weight Cycling” – Find consistency in your healthy lifestyle changes. Make sustainable modifications to your diet and exercise plan.
Reduce or Eliminate Refined Carbohydrates – Reduce white bread, pasta and sugary drinks.
Increase Your Fiber Intake – Increase your consumption of foods like vegetables and fruits.
Become More Physically Active – The American Heart Association recommends 150 minutes of moderate physical activity per week for adults. This equates to about 30 minutes, five days per week. For children, the recommendation is 60 minutes of moderate to vigorous physical activity each day. The good news is that many of these risk factors are modifiable. You have the power to reduce your risk!
About the Author:
Jennifer Franceschelli Hosterman, DO, is a board certified internal medicine and pediatric physician who specializes in nutrition and obesity medicine at Geisinger Medical Center. She is also the Medical Director of Camp ENERGY, which is a healthy lifestyle camp for adolescents. She earned her Bachelor’s degree in cellular and molecular biology at West Chester University and completed medical school at Philadelphia College of Osteopathic Medicine. She is a strong proponent of the multi-disciplinary and family approach in the prevention and treatment of obesity.
by Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Articleby Sarah Bramblette, MSHL Summer 2023 In the final months of 2022, I experienced both the worst…
Read Article