Medically Managed Weight-Loss – A Treatment Option

By Stephanie Yeager, RD, Shannon McShea, PA-C,
Laura Smith, CRNP, and Christopher D. Still, DO
Spring 2006
The Center for Nutrition and Weight Management at Geisinger Medical Center is designed to provide treatment to patients who are suffering from obesity with assistance, support and treatment for weight and weight-related problems such as heart disease and stroke, high blood pressure, sleep apnea, joint disease/limited mobility, high cholesterol, high triglycerides, low levels of HDL (high-density lipoprotein – the “good” cholesterol), and type 2 diabetes. Fortunately, even modest reductions in weight can help improve these conditions. A weight-loss of 5 to 15 percent of body weight may improve health and quality of life and prevent (or treat) these health problems. For a 200 pound individual, this would equate to a 10 to 30 pound weight-loss.
The Initial Consult
Weight management is a partnership between the patient, their family and healthcare team; comprised of doctors, nurses and dietitians. This partnership is one that is developed on an individual basis with each patient. A physician, physician assistant or nurse practitioner, specializing in obesity treatment, provides the initial consultation. The initial consult involves a focused medical evaluation for diseases related to obesity, a weight history, including past diet attempts, and a thorough psychological history. Several blood tests are often drawn; many patients come to the clinic with undiagnosed diabetes, high cholesterol, thyroid disorders or abnormal liver tests.
Management of obesity includes diet, exercise, behavior modification and psychological counseling. In certain cases, medication for weight-loss (pharmacotherapy), supervised very-low calorie diets, full/partial liquid diets or weight-loss surgery may be options (surgery and liquid diets will be addressed in future articles).
Diet and Behavior Modifications
After the initial assessment, many of the follow-up appointments are with registered dietitians or mid-level providers who are certified in obesity management, as well as exercise. Although many factors influence weight, the principal concept of the energy balance equation: “energy in, versus energy out,” is the core of the program. To lose weight, you must consume fewer calories than you burn. This is, of course, easier said than done. No matter what weight-loss methods you may employ (diet, exercise, medication or surgery), the principle of energy balance is unavoidable.
Caloric expenditure is a key component to the energy balance. In general, calorie estimation equations are not as accurate for patients who are affected by obesity or those who have lost and gained weight with dieting for many years. We offer an objective test with the use of an indirect calorimeter called MedGem®, which actually determines how many calories are burned at rest throughout the day. This is a true measurement of caloric expenditure and, thus, supplies an objective value from which the dietitian and patient can develop a realistic meal plan, which should result in weight-loss.
Getting a handle on eating behaviors is key to making significant long-term change. While no one likes to keep food logs that require writing down all food eaten, this exercise has been shown to be important for long-term success. With all the variation in serving sizes, most individuals do not have a good understanding of how many calories are actually consumed in one day. Therefore, it is recommended that, for at least the first six to eight weeks, individuals keep a complete food log. This will also help dietitians get a better handle on areas of the diet to focus at follow-up visits.
Dietitians also work with patients using individualized meal plans for various lifestyles and medical conditions. Many medical conditions, such as insulin resistance, can make it difficult to lose weight on traditional low fat diets. The dietitian can work individually with the patient to find a meal plan that will work for him or her. Also, the dietitians teach patients how to actually make the changes such as: how to shop; cooking ideas such as easy preparation methods or healthy recipes; and how to eat out at restaurants.
Our approach to weight-loss is focused more on teaching and reinforcing the importance of behavior and lifestyle changes than on “following a diet.” Many people can follow a diet and lose weight, the challenge, however, comes in maintaining the weight-loss. Our belief is that teaching behavior change facilitates lifelong success with weight-loss. Any changes in eating and exercising behaviors must become habitual, which takes time. We offer monthly visits that provide behavior modification help (strategies to help change habits) that encompass things such as record keeping; eating behavior and associated activities; eating slowly and portion control; vitamins, minerals, fiber and water; enhancing exercise; attitudes, self-esteem and quality of life; holiday eating; and stress eating.
Follow-up Visits
Patients are given the opportunity to revisit a topic or obtain more information on an area of interest during follow-up visits. The frequency of and interval between follow-up visits is determined on a patient-by-patient basis. We encourage monthly visits until initial weight-loss goals (5 to 20 percent) are achieved. At that point, we encourage every three, six or 12-month follow-up visits as needed for individual patients.
Many studies have shown that accountability is one of the major factors influencing the ability of individuals to maintain long-term weight-loss. For this reason, patients are offered and encouraged to follow-up in our clinic indefinitely. Obesity is not a disease that’s conquered in a day, month or year. It is a disease that must be fought everyday for the rest of one’s life. This combination of specialized healthcare professionals and individualized treatment plans ensures that each patient’s health is improving with steady weight reduction and weight maintenance.
Weekly weigh-ins are a useful tool to hold individuals accountable. Patients are frequently given a meal and exercise plan by their healthcare provider and told to return in two to three months. However, getting weighed on a weekly basis, at the same time and day of the week and using the same scale helps to keep dieters on track. Just knowing there will be a weekly weigh-in decreases caloric consumption. On the other hand, daily weigh-ins are not recommended since small, incremental changes often cause frustration and result in failure. It is also recommended (if possible) that the weekly weigh-in occur outside of the home. Being weighed in the presence of another person increases accountability and has been shown to decrease caloric intake per week by nearly 20 percent.
Dealing with Plateaus
We also will use the MedGem® in the case of a plateau of weight. Unfortunately, as we lose weight, our metabolism decreases. Having the ability to actually test caloric needs can be very useful in these instances. Body composition is also tested to determine actual muscle mass. This enables patients to focus on muscle mass as an objective or goal rather than the weight on the scale. Another way we deal with plateaus is to encourage an increase in both cardiovascular and muscle building exercises. The only safe and effective way to maintain one’s metabolism is by increasing or maintaining lean body mass. The most beneficial way to do this is through modest, regular exercise.
If one is able, simple walking is very beneficial. Not only does this maintain lean body mass and maintain metabolism, but it also increases bone density. Individuals who are unable to walk (due to arthritis or other problems) can use upper body exercises while seated. A simple exercise such as repetitively raising two cans of soup over the head is an exercise that can help to maintain lean body mass while burning calories.
It is important to start an exercise program slowly and build gradually. For some patients, walking two to three minutes several times each day, and then gradually increasing to 10 minutes three times a day (or 30 minutes over 24 hours) is very helpful. This 150 minutes over a seven-day period is the recommended amount of physical activity to maintain lean body mass and increase calories burned.
Medications (Pharmacotherapy)
Currently there are three medications that are FDA approved for weight-loss: sibutamine (Meridia ®), orlistat (Xenical ®) and Noradrenergics products. All are to be used in conjunction with a reduced-calorie diet, exercise and behavior modification. Pharmacotherapy should be reserved for patients with a body mass index (BMI) greater than 30 or a BMI greater than 27 with at least one cardiac risk factor (high blood pressure, high cholesterol, diabetes). A novel medication (rimonabant) has just been approved for weight-loss by the FDA in February of this year. This medication is aimed at improving cardiometabolic risk factors and assisting with weight-loss and possibly smoking cessation.
Types of Medications for Weight-Loss:
Noradregenics
Phentermine is the most commonly prescribed amphetamine-like medication for weight-loss. Phentermine is only approved for short-term use (less than 12 weeks) in adults; at that point the majority of the patients may have developed a tolerance for the drug and it is no longer as effective. This class of medications are mild stimulants that suppress appetite by altering chemical signals in the brain. Common side effects include jitteriness, dry mouth, constipation, elevated blood pressure and increased pulse rate. It should not be used in people with a history of heart disease, uncontrolled high blood pressure, seizures, or anxiety disorders.
Sibutramine
Sibutamine has been FDA approved for adults since 1999 for weight-loss and maintenance of weight-loss. It also works with brain chemicals (serotonin and norepinephrine) to help patients feel full quicker and decrease cravings for food. Similar side effects are seen with sibutamine and phentermine (listed above). Patients with poorly controlled blood pressure, heart disease, arrhythmias, heart failure, and stroke should not use sibutamine. Medications may interact with sibutamine including many antidepressants, pain medications, some antibiotics and herbal remedies. It is important that the patient tells his or her provider all medications they are taking, including over-the-counter medication and supplements.
Orlistat
In 1998, orlistat was FDA approved for weight-loss in adults and the next year was approved in teens (ages 12 and older). Orlistat is the first non-centrally acting medication that works by decreasing the absorption of fat from the intestines. Orlistat “blocks” approximately 1/3 of fat from the food eaten. Overall, Orlistat is a safe medication. It interacts with few medications (caution with warfarin and cyclosporine) and can be used in most every patient. Patients should be advised to take a multivitamin with chronic use of orlistat due to a potential decreased absorption of fat-soluble vitamins. Side effects of orlistat include diarrhea, gas, oily stools, and fecal incontinence. These side effects lessen over time and can be avoided by following a low-fat diet.
Does My Insurance Cover Medically Managed Weight-Loss?
Most insurance companies will cover office visits with providers (i.e. physician, physician assistant and nurse practitioners). It is important for the provider to document co-related medical problems caused by obesity.
Appointments with registered dietitians are not always covered by health insurance. If a patient has obesity with diabetes or kidney failure, the dietitian visits are covered by most insurers, but usually limited to how many visits are allowed per year. If a patient does have to pay for a visit, a typical dietitian appointment costs approximately $50-$75 for an initial appointment and $15-$30 dollars for a return visit.
If the patient has psychology coverage through their health insurances, then psychology visits are covered. If uncovered, this again could be an out of pocket cost to the patient. An initial psychology visit may cost around $200. Medicare/Medicaid and many other insurances carriers have the availability of covering psychology related visits.
Referrals to Other Services
Psychology
Obesity is a disease that affects more than just blood pressure, blood sugar and knee pain. It can be an enormous contributor to psychological issues, including low self-esteem, depression and relationship difficulties. Including a psychologist in the “weight management team” can be priceless. A psychologist can help patients with behavior modification and goal setting such as: finding other coping measures and alternatives to stress/emotional eating, enlisting social support, self-monitoring, relapse prevention and body image issues.
Support Groups
Support groups focusing on lifestyle, quality of life and behavior rather than food are ideal for success with weight-loss. Because our clinic is in a rural area and many patients travel hours to come to our clinic for support, we encourage joining a support group system such as Overeaters Anonymous and Take Off Pounds Sensibly (TOPS) that are usually closer to home. We also encourage the use of online support groups particularly those that are “monitored-loosely” by our staff members.
Realistic Expectations
Unrealistic goals of a comprehensive weight management program often result in failure. Therapy should not be expected to achieve the “ideal” body weight often set as a measure of success. A modest weight-loss can offer profound benefit in preventing or delaying the onset of co-morbid medical problems and should be viewed as a success. This realistic goal of a 10 to 15 percent weight-loss from initial weight will keep one focused, as well as improve their quality of life and help manage any obesity co-morbid medical problems.
About the Authors:
Shannon McShea, PA-C, is a Physician Assistant at Geisinger Medical Center in Danville, Pennsylvania. She has worked within the Center of Nutrition and Weight Management for the last five years. She earned her bachelor’s degree in nutrition science from Penn State University and her masters from DeSales University. She is part of a multidisciplinary team that treats those individuals affected by obesity and their co-morbid medical problems through diet, exercise and/or pharmacotherapy and bariatric surgery.
Laura Smith, CRNP, is a Nurse Practitioner at Geisinger Medical Center in Danville, Pennsylvania. She has worked within the Center of Nutrition and Weight Management for the last year. She earned her bachelor’s degree in nutrition science from Purdue University and her masters from Bloomsburg University. She is part of a multidisciplinary team that treats those affected by obesity and their co-morbid medical problems through diet, exercise, and/or pharmacotherapy and bariatric surgery
Christopher D. Still, DO, FACP, FACN, has been studying developments in nutrition support and obesity for nearly a decade. He serves as principal investigator on a rural elderly nutrition and aging study of some 22,000 individuals. Dr. Still’s interest in weight-loss comes from his personal experiences with obesity. Dr. Still once weighed 365 pounds, and losing the weight was a life and career changing experience. Dr. Still is certified by the American Board of Internal Medicine, the American Board of Nutrition and the American College of Nutrition, among others. He is also a member of the OAC Board of Directors.
Stephanie F. Yeager, RD, LDN, is a Registered Dietitian at Geisinger Medical Center in Danville, Pennsylvania. She has worked within the Center for Nutrition and Weight Management for the last four years. She received her bachelor’s degree in nutrition science from Penn State University. She specializes in weight management and exercise. She is part of a multidisciplinary team that treats those affected by obesity and their co-morbid medical problems through diet, exercise, and/or pharmacotherapy and bariatric surgery.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
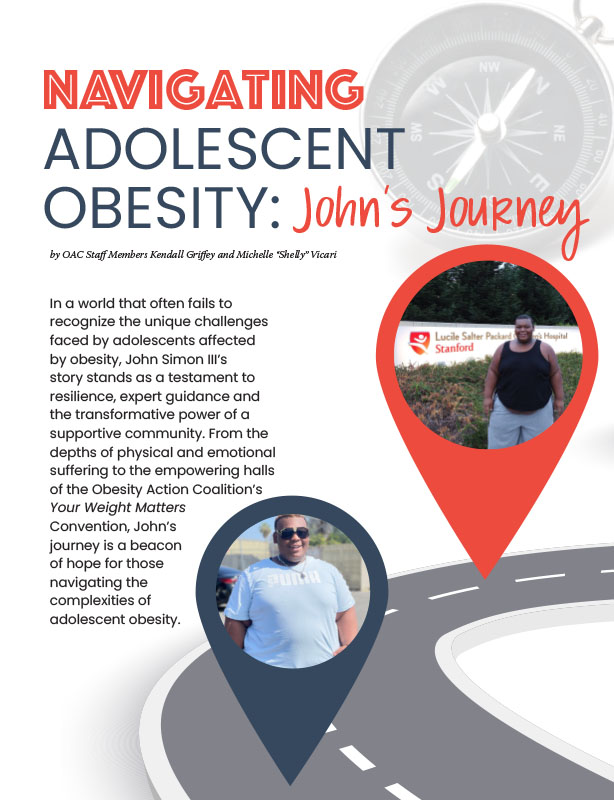
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article