How Does Bariatric Surgery Resolve Diabetes?

by Stephen G. Boyce, MD, FACS
Fall 2017
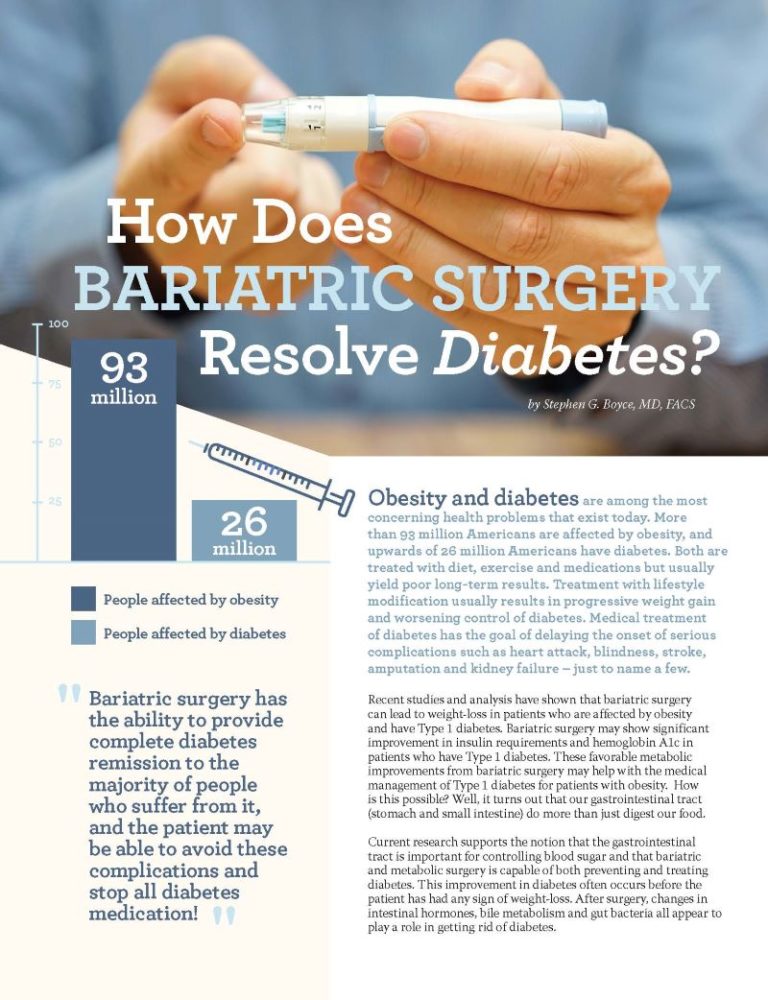
Obesity and diabetes are among the most concerning health problems that exist today. More than 93 million Americans are affected by obesity, and upwards of 26 million Americans have diabetes. Both are treated with diet, exercise and medications but usually yield poor long-term results. Treatment with lifestyle modification usually results in progressive weight gain and worsening control of diabetes. Medical treatment of diabetes has the goal of delaying the onset of serious complications such as heart attack, blindness, stroke, amputation and kidney failure – just to name a few.
Recent studies and analysis have shown that bariatric surgery can lead to weight-loss in patients who are affected by obesity and have Type 1 diabetes. Bariatric surgery may show significant improvement in insulin requirements and hemoglobin A1c in patients who have Type 1 diabetes. These favorable metabolic improvements from bariatric surgery may help with the medical management of Type 1 diabetes for patients with obesity. How is this possible? Well, it turns out that our gastrointestinal tract (stomach and small intestine) do more than just digest our food.
Current research supports the notion that the gastrointestinal tract is important for controlling blood sugar and that bariatric and metabolic surgery is capable of both preventing and treating diabetes. This improvement in diabetes often occurs before the patient has had any sign of weight-loss. After surgery, changes in intestinal hormones, bile metabolism and gut bacteria all appear to play a role in getting rid of diabetes.
Mechanism of Diabetes Remission after Bariatric Surgery
Although we know that the gastrointestinal tract produces more than 100 known hormones, the exact way it resolves diabetes is not fully understood. What we have learned is that there are several mechanisms that come into play, including:
-
- Starvation
- Stomach
- Upper and lower part of the small intestines
These “parts” of the intestinal tract play a role in resolving diabetes after bariatric surgery by removing hormones that stimulate appetite, bypassing parts of the intestines so that they do not “see food” and by delivering food to the lower part of the intestines rapidly after eating.
Starvation
After bariatric surgery, patients usually consume about 400-500 calories per day. This is less than the patient’s metabolic rate and is, in effect, starvation. This produces rapid weight-loss and assists with diabetes resolution. Starvation begins the process of reversing insulin resistance. With starvation and weight-loss, the liver and skeletal muscle cells lose fat from inside the cell which makes them more sensitive to insulin.
Weight-loss with starvation takes time, and for 50 years, bariatric surgeons have noticed that their patients’ diabetes often resolves immediately after surgery – before the patient has had any significant weight-loss. Additionally, if starvation were the only cause of diabetes resolution, one would think that gastric banding would have similar rates of diabetes remission as the gastric bypass and duodenal switch. However, diabetes only resolves 48 percent of the time after banding, but resolves 84 percent of the time with gastric bypass and 95 percent of the time with duodenal switch. Clearly there is more to diabetes resolution after bariatric surgery than the effects of starvation alone.
The Stomach
The stomach produces hormones that are involved in glucose regulation, such as Ghrelin, Gastrin and Glucose-dependent insulinotropic polypeptide (GIP).
Ghrelin is made primarily in the top part of the stomach. It is the only known appetite-stimulating hormone in the body, and it also acts to reduce insulin secretion after a meal. The stomach usually makes Ghrelin in large amounts before a meal, and then after eating, the Ghrelin production is greatly reduced. After bariatric surgeries such as sleeve gastrectomy and gastric bypass, Ghrelin levels drop up to 75 percent – causing patients to have a reduced appetite, secrete more insulin and have lower blood sugar levels.
Gastrin is produced in the lower part of the stomach (but also by the small intestines and pancreas) after eating. Gastrin makes a patient feel full by stimulating the pancreas to make more insulin after a person eats a meal. This also has the effect of improving diabetes.
Glucose-dependent insulinotropic polypeptide (GIP) levels are elevated after gastric bypass and cause the pancreas to release more insulin. This causes the liver and muscle cells to remove glucose from the blood stream and produce lower blood sugar levels.
The Upper Intestine Theory
The upper intestine theory proposes that by bypassing the upper part of the small intestine, diabetes improves because specialized endocrine cells secrete anti-diabetic compounds in the absence of food. Endocrine cells perform a process in which a group of cells secretes into the blood or lymph circulation a substance (for example, hormone) that has a specific effect on tissues in another part of the body. Anti-diabetic compounds help cells metabolize glucose, as well as lipids and proteins, and combat insulin resistance.
Support for this theory comes from an operation called the duodenojejunal bypass (DJB). DJB involves bypassing the first three feet of the small intestine. After DJB, there isn’t any weight-loss, but rapid improvement in diabetes and a reduction in hemoglobin A1c (HbA1c) has been shown, which is a strong marker of diabetes. If you reverse the DJB, the diabetes returns. This indicates that if you bypass the upper small intestine, you block signals that promote diabetes. These signals or compounds from the upper small intestine have not been identified yet.
Specialized endocrine cells such as glucagon is a hormone that can be used to treat severe low blood sugar. Glucagon-like peptide-1 is a 30-amino acid long peptide hormone deriving from the tissue-specific posttranslational processing of the proglucagon gene. Oxyntomodulin is a naturally occurring 30-amino acid peptide hormone found in the colon, produced by the oxyntic (fundic) cells of the oxyntic (fundic) mucosa. It has been found to suppress appetite. Amino acids serve as the building blocks of polypeptides, and polypeptides serve as the building blocks of proteins.
The Lower Intestine Theory
The lower intestine theory suggests that by getting food to the lower intestine more quickly (by bypassing the upper intestine), diabetes is improved. Operations that best improve diabetes are gastric bypass and duodenal switch, which create a shortcut for food to get to the lower intestine. When undigested food gets to the lower intestine, it causes specialized endocrine cells to secrete glucagon like polypeptide 1 (GLP 1), oxyntomodulin (OXM) and polypeptide YY (PYY) among others.
GLP 1 is elevated after bariatric surgery, causing the pancreas to secrete more insulin. This has been shown to help the pancreas cells which make insulin (beta cells) revive after damage from diabetes.
OXM improves diabetes by causing intestinal cells to remove sugar from the blood stream, causing people to burn more energy through improved metabolism and reduced appetite due to satiety.
PYY appears to improve diabetes by stimulating the brain to release a hormone called alpha MSH that decreases appetite. PYY is elevated after bariatric surgery.
Conclusion
In summary, bariatric surgery has the amazing ability to prevent and treat diabetes! It does so at least in part by altering intestinal “hormones” that cause the pancreas to secrete more insulin and cause the body to be more sensitive to insulin. The anti-diabetic effects are proven to be more effective than the best medicines available.
About the Author:
Stephen Boyce, MD, obtained his Bachelor of Science and Masters of Science from Texas A&M University and medical school at the University of Texas Southwestern Medical School. Dr. Boyce has completed more than 4,000 bariatric surgical procedures, special training in advanced laparoscopic surgery and has also completed a Masters Certification in Bariatric Surgery. He started his own practice, the New Life Center for Bariatric Surgery, in Knoxville, Tenn. in 2002, which became one of the Nation’s first Centers of Excellence (7th in the Nation) in 2005. His special interest in bariatric nutrition led him to develop Bari Life Bariatric Supplements. Additionally, he is an active educator for Ethicon-Endo Surgery and a two-time recipient of the OAC’s Dr. Blackstone Outstanding Membership Recruitment by a Physician award.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
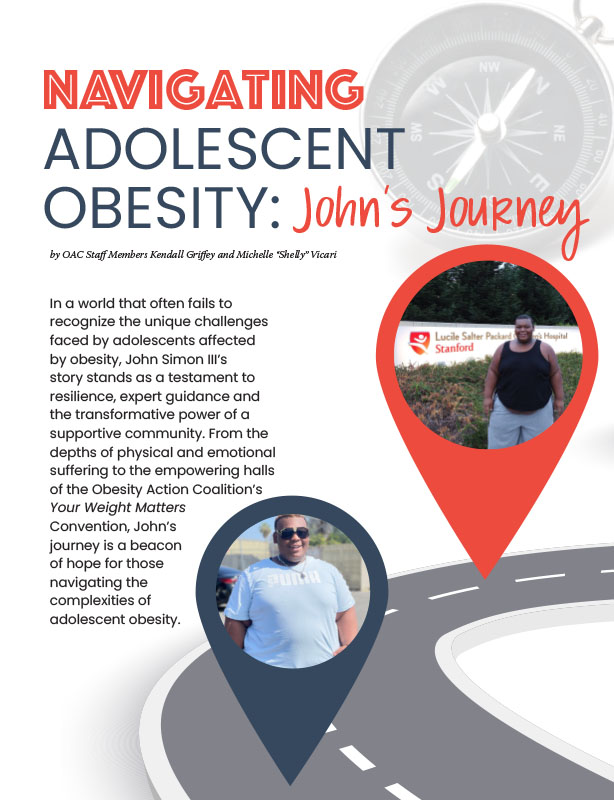
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Article