Ghrelin, the “Go” Hormone

by Ted Kyle, RPh, MBA, and William Hignett
Fall 2011
What if we could, for one day, create our bodies and change them as we please to improve our physical nature? How would we enhance our strengths and address what we see as problems? How would we change our bodies and minds to alleviate stress, anxiety and physical problems? Related to weight, we would probably make it easier and very straightforward to lose pounds and fat and to keep the weight off our bodies.
If we had this power, we might consider simplifying hormonal actions that fuel and curb hunger so these actions are clear-cut and we comprehend exactly how to lose weight. In fact, in real life, two hormones do appear to be this direct in their actions on eating and weight. Ghrelin (grell-in) is the hunger hormone and leptin is the stop appetite hormone. Many believe that the actions of these “go and stop” appetite hormones are straightforward, and that one is bad and the other is good.
Ghrelin, the “Hunger Hormone”
Ghrelin is responsible for stimulating hunger, and it is the “go” hormone that tells you when to eat. As the “hunger hormone,” some may be ready to make ghrelin out to be a villain. Obesity and weight-loss are complicated, so perhaps it would be comforting to have a bad guy hormone that stimulates hunger so we can focus on this “bad” hormone that causes us to gain weight.
Interesting Fact
What exactly is meant by saying ghrelin is the hunger hormone? The ghrelin hormone, discovered in 1999, is released primarily from cells in the stomach and travels to the brain. There, it interacts with both the hypothalamus (the brain’s physiological eating center) and the brain’s pleasure centers to arouse hunger.
Throughout the course of a day, ghrelin levels naturally change dramatically, rising steeply before a meal and then plummeting after eating. Ghrelin stimulates the brain, which leads to an increase in appetite, and it slows metabolism and decreases the body’s ability to burn fat. Ghrelin also favors the amassing of fatty tissue in the abdominal area. In experiments, people who got injections of ghrelin before a buffet meal ate 30 percent more than a group of eaters not given extra ghrelin.
Like many things in life, it is not as apparent as it seems that ghrelin is a hunger hormone and therefore bad. Consider, for example, that ghrelin levels in the blood of individuals affected by obesity are lower than those in leaner individuals. That finding is opposite to expectations that obesity would be due to excess levels of the hunger hormone. It has also been discovered that individuals suffering from anorexia have high blood levels of ghrelin compared to both the thin and normal-weight controls.
The findings suggest that ghrelin is inversely related to calorie intake. Other studies have found that individuals who lose weight and try to keep it off make more ghrelin than they did before losing weight, as if their bodies are fighting to regain the lost fat. An explanation for these findings is that excess weight may increase sensitivity to ghrelin. For example, there may be more receptors in those affected by obesity for the hormone, so not as much ghrelin is needed to stimulate hunger.
Leptin, the “Stop Appetite Hormone”
The opposing hormone to ghrelin is the stop appetite hormone, leptin. Leptin is a hormone produced in the fat cells. It plays a role in regulating body weight by signaling the brain to reduce appetite and burn more calories. Leptin is a primary modulator of body weight and metabolism, and it mediates weight-loss by decreasing hunger and food consumption and increasing energy expenditure. Yet, some studies have shown that losing weight causes a marked decrease in leptin levels, which may in turn increase appetite.
Counter to what would be anticipated, obesity is linked to unusually high concentrations of leptin. Some research suggests that these high concentrations make the receptors for leptin inactive and impair the very mechanism that should eliminate excess fat. Then, although plenty of leptin is produced, the body’s appetite suppression system is unable to function properly.
Ghrelin Blockers as a Weight-loss Treatment
If ghrelin stimulates hunger, wouldn’t a ghrelin inhibitor (antagonist) be effective in helping people lose weight? Several pharmaceutical companies have or are conducting research on such a compound. The Scripps Research Institute in California in 2006 successfully developed an anti-obesity ghrelin vaccine that significantly slowed weight gain and reduced body fat in animals. It is possible that in the future there will be a ghrelin blocking medication. But, since ghrelin also makes eating food more pleasurable, a drug blocking the brain’s pleasure centers might create side effects related to mood regulation.
The research on ghrelin blockers is no slam dunk. Take as an example the promising medication, rimonabant, which works by interfering with one of the brain’s cannabinoid receptors and successfully causes weight-loss. However, rimonabant also affects the pleasure center in the brain and side effects include the potential for severe depression, sometimes leading to suicide. This drug was not approved for use due to these side effects.
Conclusion
Finally, what is not known is how important the role ghrelin plays in everyday eating and weight gain/loss. More research is needed before firm conclusions can be drawn about the effects of ghrelin. But, if we could create our bodies for one day, perhaps we’d simplify the actions of ghrelin and leptin and overcome the appetite stimulating effects of the “hunger hormone.”
Beyond this wish, the reality is that the human body has a complex system of hormones that interact in countless ways. Therefore, we are not likely to find a simple one-to-one relationship between these hormones and weight, or that ghrelin and leptin are likely part of a chain of physiological processes; too bad. We could use a villain when considering the challenges of obesity.
About the Authors:
Ted Kyle, RPh, MBA, is a pharmacist and health marketing expert. He is a member of the OAC National Board of Directors.
William Hignett is a disease management expert with a master’s degree in public health from the University of Pittsburgh. He has years of experience as a health educator for universities, hospitals, Fortune 100 companies and health insurers.
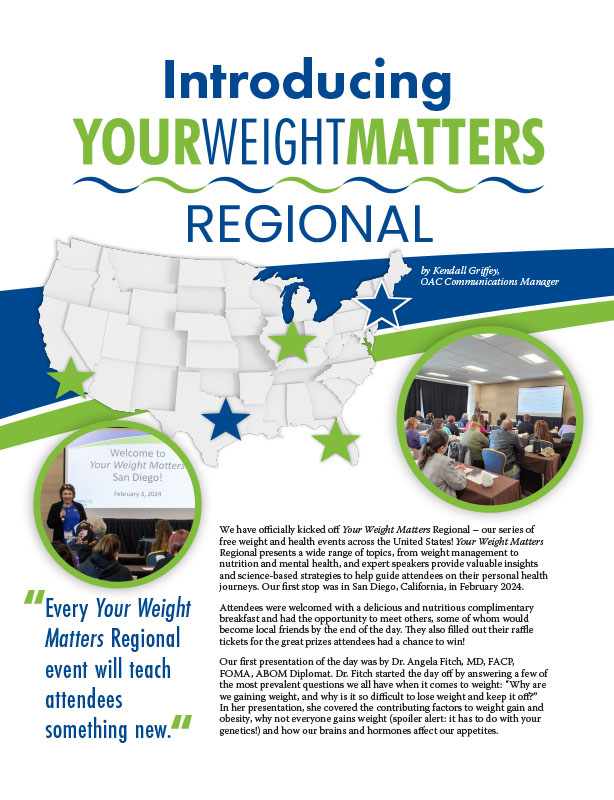
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read ArticleTelemedicine became a popular tool during the pandemic because it allows healthcare professionals to provide medical care…
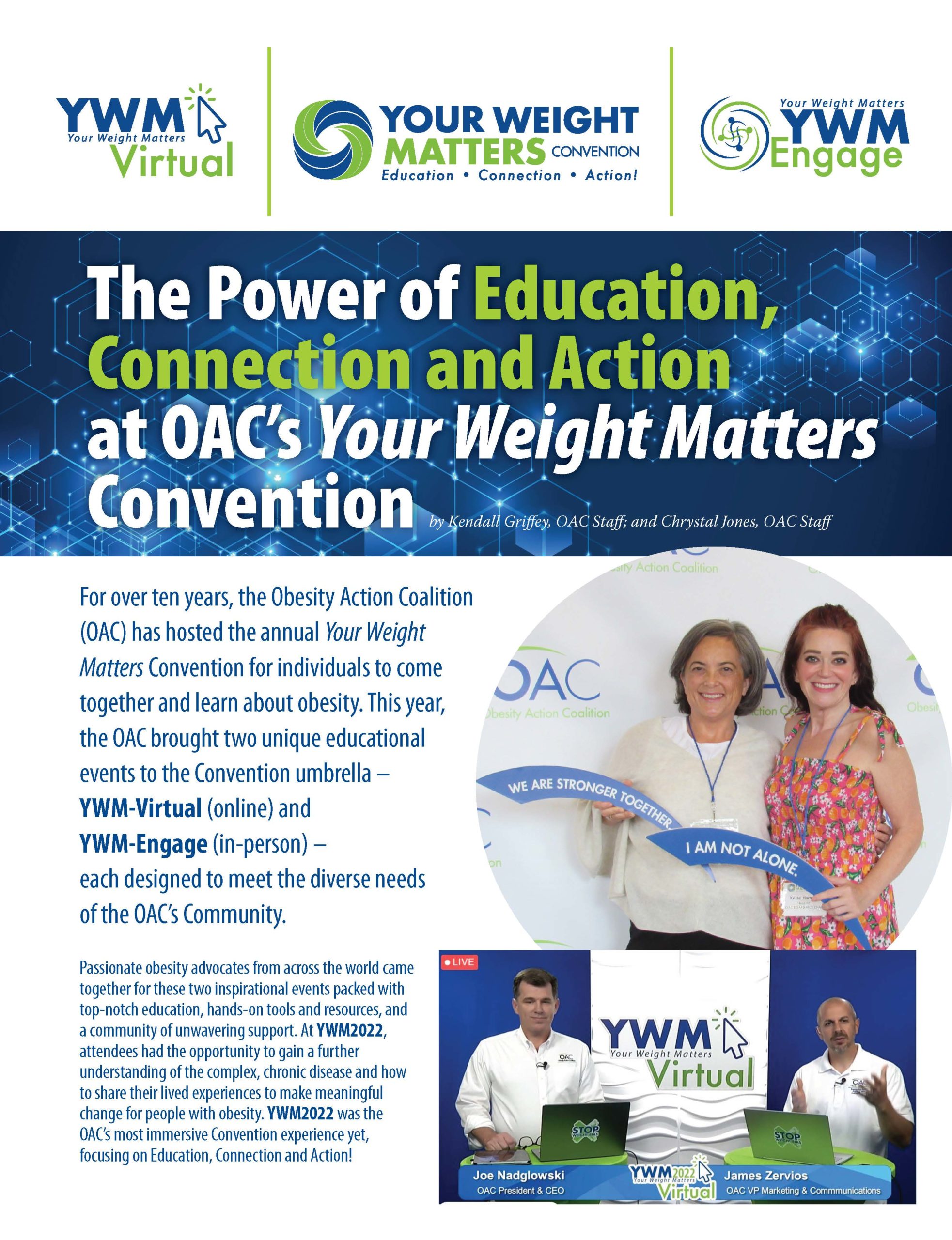
View Videoby Kendall Griffey, OAC Staff; and Chrystal Jones, OAC Staff Fall 2022 For over ten years, the…
Read Article