Access Denied: Recommended Cancer Screening

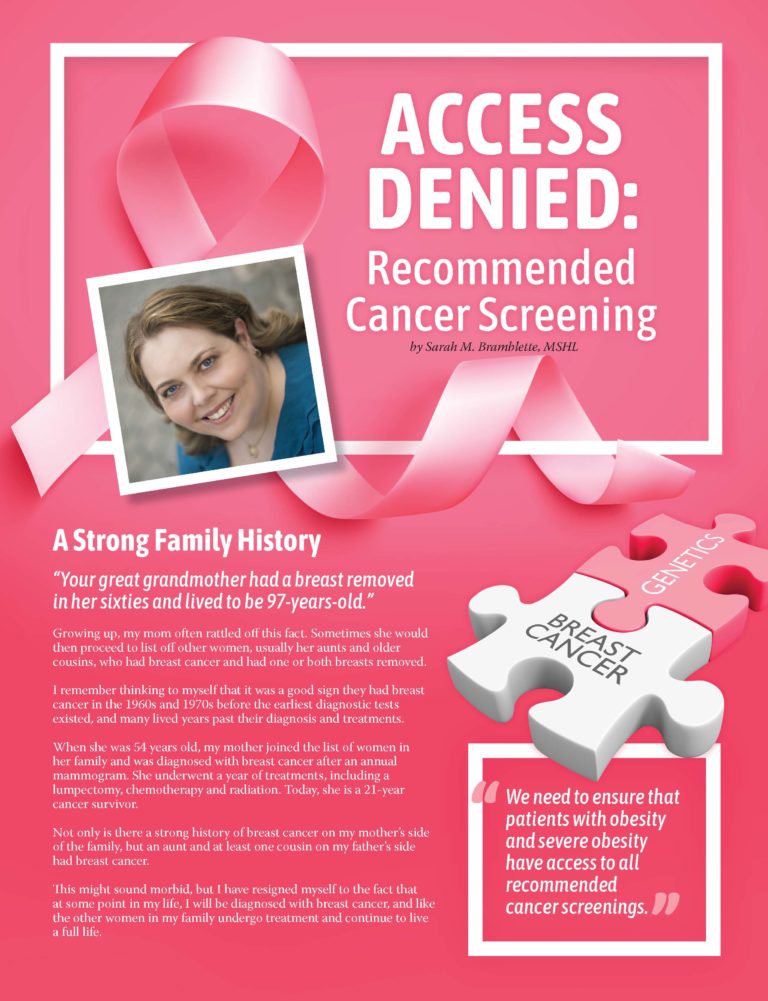
by Sarah M. Bramblette, MSHL
Spring 2022
A Strong Family History
“Your great grandmother had a breast removed in her sixties and lived to be 97-years-old.”
Growing up, my mom often rattled off this fact. Sometimes she would then proceed to list off other women, usually her aunts and older cousins, who had breast cancer and had one or both breasts removed.
I remember thinking to myself that it was a good sign they had breast cancer in the 1960s and 1970s before the earliest diagnostic tests existed, and many lived years past their diagnosis and treatments.
When she was 54 years old, my mother joined the list of women in her family and was diagnosed with breast cancer after an annual mammogram. She underwent a year of treatments, including a lumpectomy, chemotherapy and radiation. Today, she is a 21-year cancer survivor.
Not only is there a strong history of breast cancer on my mother’s side of the family, but an aunt and at least one cousin on my father’s side had breast cancer.
This might sound morbid, but I have resigned myself to the fact that at some point in my life, I will be diagnosed with breast cancer, and like the other women in my family undergo treatment and continue to live a full life.
More than Just Family
Despite having a strong family history of breast cancer, I have never had, nor has a doctor-advised genetic testing for the BRCA1 or BRCA2 gene mutation. My mother was never advised to be evaluated, and the few relatives who I know have been tested do not have the gene mutation.
I do not need a genetic test to know my family history puts me at a higher risk for developing breast cancer in my lifetime. According to the American Cancer Society, only about 5% to 10% of breast cancer cases are hereditary. There are other factors that can increase personal risk. In my case there are several: fibrocystic changes, having never given birth and severe obesity.
Knowing the importance of early detection, I have always taken my breast health seriously. In my late 20s, I had some tenderness in my right breast and I could feel a very small lump. I told my Primary Care Physician who confirmed with a physical breast exam and ordered additional testing. Due to my age, an ultrasound was recommended instead of a mammogram. The ultrasound detected a tiny cyst, which was aspirated, and results showed it was benign.
During the aspiration procedure, the radiologist asked me if I was aware that my weight put me at a higher risk for breast cancer and told me I should consider trying to lose weight. I was annoyed by her comment and told her I was working on it. At the time, I weighed approximately 280lbs, having lost nearly half my body weight after Roux-en-Y gastric bypass, a surgery which she should have reviewed in my medical history.
As is common after significant weight-loss, I had several reconstructive surgeries to remove excess skin, including a breast lift. I made the decision not to get breast implants as I knew they could interfere with mammograms. However, any breast surgery might affect diagnostic tests.
My First Mammogram
A month after my 40th birthday, I asked my PCP if I could go ahead and get my first mammogram or wait until my annual check-up, which was not due for another five months. My PCP ordered a screening mammogram and since I have Medicare as my insurance, it covered a newer type of mammogram called digital breast tomosynthesis, or 3D mammography. 3D mammography potentially finds more breast cancers than 2D. However, more studies are being done to compare the results. It was a relief to know that I had access to a potentially better-quality mammogram.
On the day of the appointment, the facility staff asked me to complete several pages of paperwork which included questions about family history, my personal history, my current health status and any current breast symptoms. I was asked to change into a robe for the test, but the available robes did not fit me, so I was unable to change before going into the actual exam room. Once inside, I removed my top and had both breasts exposed while the technician positioned me for the various images. Sadly, I am used to not having gowns available that fit me. While it bothers me, not wearing a robe did not affect the results of the screening.
What Happened Next Bothered Me
The results of my first mammogram stated, “there is no radiographic evidence of malignancy,” so the good news was there were no signs of cancer. However, there was an additional note: “given the family history of breast cancer, bilateral breast MRI with contrast is recommended.”
Despite knowing how important early detection is, I had some initial hesitation about having another test done. I asked my PCP if she thought a breast MRI was necessary and she explained that The American Cancer Society recommends an annual MRI if the lifetime calculated risk of breast cancer on any model is 20% (due to family history, other personal risk factors, genetic mutations, etc.). My lifetime risk was calculated at 25%. She recommended I get the MRI since an MRI is more likely to detect cancer than a mammogram.
Fortunately, I knew the facility where I had my mammogram also had an MRI machine with the weight capacity since they listed the information on their website. However, when I called to schedule my appointment, the scheduler told me that breast MRIs are only done at the main hospital. I asked what the weight capacity was for the machine and she said it was 495 lbs.
A day before my appointment, I called to reschedule and to my shock, was told that the appointment should never have been made because the hospital MRI machine for breast MRIs has a weight capacity of 250 lbs. I was over the capacity. I would have been very upset to find that out upon arrival for an appointment. It not only would have been a waste of my time, but a waste of the facility and staff’s time to have an appointment slot go unfilled.
Better Understanding the Problem
Knowing there were MRI machines with higher weight capacities available, I sent an email to the hospital system patient relations department to ask if it would be possible to have a breast MRI performed on one of the other machines. I received a detailed response from the MRI center explaining the reasons why I would not be able to have the MRI. The concern is not only one of machine weight capacity, but also space. The apparatus patients must be positioned on for the procedure limits the space inside the machine.
Luckily, my mammogram was clear, but what if I needed an MRI for further examination of an area? Research shows that individuals with obesity are at a higher risk for developing many cancers, so why are recommended screenings not accessible for patients who weigh more than 300 lbs.? I applaud the hospital for having an MRI machine with 495 lbs. and 650 lbs. weight capacities, but it is very disappointing that those machines are not available for a breast MRI. We need to ensure that patients with obesity and severe obesity have access to all recommended cancer screenings. Treatment for obesity is not enough. We must be able to accommodate all patients.
A Note from OAC Partner
“We recognize that the process of having an MRI can be intimidating, especially if it’s a patient’s first time having one. Unfortunately, not all scanners on the market can accommodate all patient body types at this time. We at Fujifilm are continually working to improve the patient experience through patient insights, provider knowledge and working with organizations such as the Obesity Action Coalition. Fujifilm MRI and CT scanners feature larger openings, higher table weights and amenities to address the broadest range of body types. Imaging centers and hospitals all over the world use our equipment to ensure the best patient experience while providing the ordering physicians the results to complete patient care. Our unique Open MRI scanner, Velocity, can accommodate patients up to 660 lbs. and our Oval scanner features the widest opening for systems in its class. Our Scenaria View CT scanner has an 80 cm opening and can accommodate patients up to 550 lbs. Fujifilm remains dedicated to caring for patients of all sizes and will continue leading the imaging field in innovation and patient accommodation.”
– Tracy Ricchiuto, BA, RT (R) (MR)
Product Manager, MRI
Product Marketing
About the Author:
Sarah M. Bramblette, MSHL is a member of the Obesity Action Coalition (OAC) Board of Directors and Co-chair of the OAC Access to Care Committee. She also serves as Board Chair of the Lymphedema Advocacy Group. As a patient living with obesity, as well as both Lipedema and Lymphedema, she shares her story to spread awareness about her conditions while advocating for improved diagnosis, treatment and insurance coverage for obesity and fat disorders that are often mistaken for obesity.
by Nina Crowley, PhD, RD (with Inspiration from Shawn Cochran) Winter 2024 Dating, no matter your age,…
Read Articleby Leslie M. Golden, MD, MPH, ABOM Diplomate Winter 2024 The journey to overcoming obesity is a…
Read Articleby Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Article