Obesity and Heart Disease


by Sunil Daniel, MD
Summer 2015
Obesity is a complex, chronic disease that should be properly assessed and treated seriously. It is second only to smoking tobacco as the leading cause of preventable death in the United States. According to Center for Disease Control and Prevention (CDC), in 2011-2012 more than one-third of adults (34.9 percent) and one-sixth (16.9 percent) of children and adolescents in the United States were affected by obesity.
Obesity is defined as having a body mass index (BMI) equal or greater than 30 kg/m2 which increases the risk for multiple chronic conditions such as type 2 diabetes, hypertension, heart disease, musculoskeletal disease, cancer, obstructive sleep apnea, kidney disease and abnormal cholesterol, among other health conditions. These chronic conditions not only have a great impact on the quality of an individual’s life, but they also contribute to higher healthcare cost and decreased work productivity.
According to World Health Organization, Cardiovascular Disease (CVD), defined as disorders of the heart and blood vessels, is the number one cause of death globally. Multiple risk factors contribute to CVD. These can be divided into modifiable and non-modifiable risk factors:
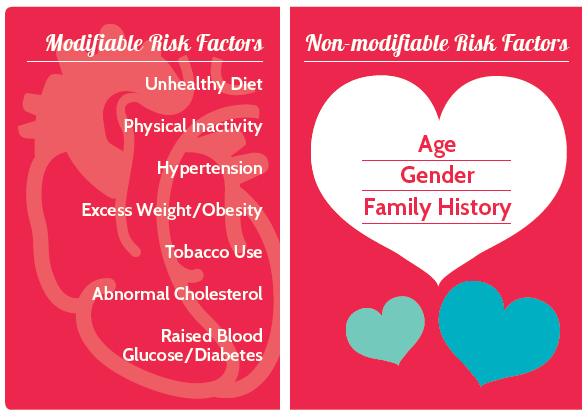
Obesity is an independent risk factor for CVD, negatively affecting the heart’s function and structure as well as the blood vessels’ inner lining. Obesity affects the heart through risk factors, such as:
- Hypertension
- Obstructive Sleep Apnea
- Elevated Blood Glucose
- Inflammation
Therefore, obesity has a major influence on CVD, contributing to symptoms such as heart failure, atrial fibrillation, coronary heart disease, stroke and venous thromboembolism.
Heart Failure
Based on National Health and Nutrition Examination Survey (NHANES) 2007-2010 survey data, about 5.1 million Americans 20 years of age or older in United States have heart failure. In 2009, 7.2 percent of deaths were due to heart failure. A higher BMI is associated with increased risk of heart failure–for every one unit of increase in BMI, the risk of heart failure increases by 5 and 7 percent in men and women respectively.
As body weight increases, its total blood volume and the amount of blood pushed by the heart into the body also increases, resulting in increased cardiac output. The increase in the body’s total blood volume also increases the volume of blood that returns to the heart, leading to dilation and enlargement of the right and left ventricle and increasing wall tension. Throughout time, the muscle wall of the left ventricle thickens, known as left ventricular hypertrophy, and this leads to heart failure. In right heart failure, the heart cannot pump blood to the lung for oxygenation, and in left heart failure, the heart cannot pump enough oxygenated blood to the body.
Atrial Fibrillation
Atrial Fibrillation (AF) is the most common type of arrhythmia, an abnormal heart rate or heartbeat rhythm. Under normal conditions, the upper and lower chambers of the heart contract and relax in a synchronized fashion to move blood from the upper to lower chambers, and pump blood out to the lungs and body. During AF, the upper and lower chambers of the heart are not synchronized. The upper chambers beat irregularly and too fast, resulting in ineffective transfer of blood into the lower chambers and out to the body. This also contributes to the slowing of blood flow and an increased risk of blood clot formation that, if pumped out of the heart, can travel to the brain, resulting in stroke.
Affecting three million Americans in 2005, AF has been projected to reach eight million by the year 2050. While increase in age, medical history of coronary heart disease, hypertension and heart failure predispose an individual to AF, obesity is also a major risk factor. One study showed that obesity increases the risk of developing AF by 49 percent, and the risk increases with a higher BMI.
Coronary Heart Disease
Based on NHANES 2007-2010 survey data, 15.4 million Americans above 20 years of age have Coronary Heart Disease (CHD). In 2009, CHD accounted for 49 percent of deaths due to cardiovascular disease. Atherosclerosis, plaque deposits on the inner walls of the blood vessel, is the cause of coronary heart disease. Plaque is made up of cholesterol, calcium, clotting material, and other substances. As the plaque builds up in blood vessels of the heart, it can partially or completely block the flow of the blood to the heart. This results in decreased delivery of oxygen to the heart muscles, causing chest pain (angina) and/or a heart attack. Plaque deposition and build-up is a slow process, and it can start in individuals as young as 5 to 10 years of age. In general, obesity and excess fat around the abdominal area is associated with increased atherosclerosis. One study showed that obesity in adolescents and young adults accelerates the progression of atherosclerosis.
Stroke
Each year, 795,000 people experience a stroke, with 610,000 of them having their first attack. On average, every 40 seconds someone in United States has a stroke. Based on the NHANES 2007-2010 survey data, 6.8 million Americans above 20 years of age have had a stroke. A stroke occurs when there is lack of oxygen delivery to the brain. During this time, brain cells are very sensitive and within minutes of low or no oxygen delivery, they begin to die.
There are two types of strokes: ischemic and hemorrhagic. Ischemic stroke is the most common type of stroke, accounting for 87 percent of those experienced. It is caused by disruption to the flow of oxygenated blood to the brain. This disruption can be due to plaques or blood clots that have formed in the blood vessels that supply oxygenated blood to the brain (thrombotic stroke). The disruption of blood flow can also be caused by a plaque or blood clot that was formed outside of the brain and through blood flow lodges in narrow brain vessels.
Hemorrhagic stroke (13 percent of strokes) occurs when the blood vessel in the brain leaks or ruptures. Risk factors for stroke include hypertension, atrial fibrillation, obstructive sleep apnea, diabetes, physical inactivity and high blood cholesterol. Obesity is the common link among these risk factors.
Venous Thromboembolism
A common finding in severe obesity is leg swelling, which may be a consequence of the structural and functional effect of excess weight on the heart. Leg swelling and decreased mobility encountered in those with excess weight and obesity reduces the pumping function of the calf and leg muscles. This results in blood flow problems in the leg veins, and leads to malfunctioning of the valves in the veins. The risk of severe and sustained lower extremity venous flow problems (venous stasis) causes leg ulcers and skin infections. The risk of developing blood clots in legs, known as venous thromboembolism (VTE), and in lungs, known as pulmonary embolism, is also increased in obesity.
Weight-loss and Heart Disease
Moderate weight-loss of even 10 percent in those with excess weight and obesity can improve or even prevent obesity-related risk factors for CVD. Current therapies available for weight management include diet, physical activity, pharmacotherapy and bariatric surgery. Behavior modification to help with diet and activity is an important component of all of these treatments. A beneficial impact of weight-loss on the cardiovascular system is decreased stress on the heart, leading to improvements in its structure and function. In a major clinical trial, an Intensive Lifestyle Intervention (ILI) involving group and individual meetings to achieve and maintain weight-loss through decreased caloric intake and increased physical activity was compared to a group that received usual care and education. Dietary strategies included portion-controlled diet, liquid meal replacements, and recommendations to use other portion-controlled items to promote adherence. The exercise goal was at least 175 minutes of physical activity per week, using activities similar in intensity to brisk walking. Behavioral strategies, including self-monitoring, goal setting and problem solving were stressed.

The ILI was successful in producing sustained weight-loss and improvements in cardiovascular fitness and CVD risk factors through four years of follow-up. A significantly greater decrease in the number of medicines used to treat their diabetes and blood pressure was also seen. Several research studies provide consistent evidence that those with severe obesity undergoing bariatric surgery have lower rates of heart attacks, strokes, and other heart disease-related complications after weight-loss.
Conclusion
Recent research has brought to light a paradox showing individuals affected by excess weight or obesity (Stage 1, BMI 30-34.9) have a slight protection against serious CVD complications compared to individuals with normal weight (BMI <25) who have CVD. However, the evidence is very clear and strong that those with severe obesity (BMI > 40) carry an extremely high risk for CVD complications, including sudden death. This highlights the importance of cardiovascular fitness regardless of weight status. The American College of Sports Medicine recommends that most adults engage in moderate-intensity cardiorespiratory exercise training for more than 30 minutes per day on more than five days a week, for a total of more than 150 minutes per week. For greater weight-loss and enhanced prevention of weight regain, the recommendation is approximately 250 to 300 minutes per week of moderate-intensity physical activity.
About the Author:
Sunil Daniel, MD, is an obesity medicine physician with fellowship training in clinical nutrition and obesity management. His academic experience includes a faculty position in the Department of Nutrition Sciences at the University of Alabama at Birmingham (UAB). He has authored several scientific papers on obesity and its medical management. Dr. Daniel is a Duke University-trained Integrative Health Coach and an innovator who is passionate about developing mobile technology enabled weight-loss solutions that are both evidence-based and meaningful to the user. He takes pride in sharing with others his own success and challenges with weight-loss and weight maintenance.
by Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Articleby Sarah Bramblette, MSHL Summer 2023 In the final months of 2022, I experienced both the worst…
Read Article